New Study Shows Role of Macrophages Misunderstood in Fibrosis
DENVER —
 Researchers at National Jewish Health and colleagues have completed the first study comparing lung macrophages in multiple models of lung injury. The research indicates that macrophages previously described as “pro-fibrotic” are insufficient to cause fibrosis on their own, opening the door to research that can help advance the understanding of how macrophage programming can help or hinder lung repair. The study was recently published in the journal JCI Insight.
Researchers at National Jewish Health and colleagues have completed the first study comparing lung macrophages in multiple models of lung injury. The research indicates that macrophages previously described as “pro-fibrotic” are insufficient to cause fibrosis on their own, opening the door to research that can help advance the understanding of how macrophage programming can help or hinder lung repair. The study was recently published in the journal JCI Insight.
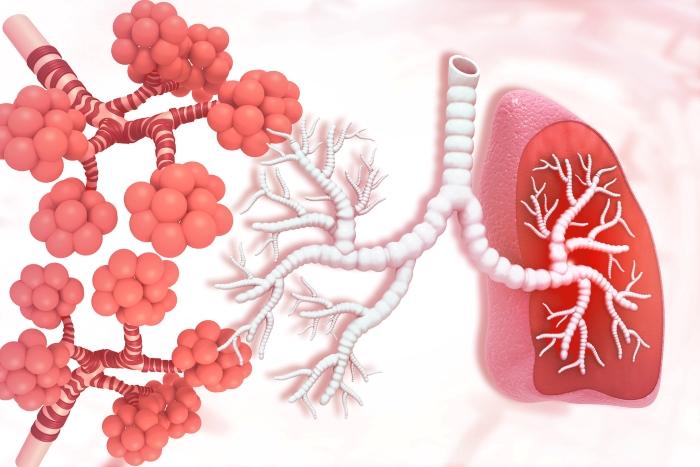
Macrophages are immune cells that reside in and protect the lungs and are also recruited to the lungs in high numbers during injury or disease. They are key to the initiation and resolution of various types of lung injuries, but also are involved in pathways that lead to lung scarring (fibrosis). It is currently unclear what mechanisms differentiate macrophages that lead to healthy repair from those that lead to fibrosis. This research sought to explore if different genetic groups of macrophages were involved in these different outcomes.
“We now know the role of macrophages have been misunderstood,” said William Janssen, MD, section head of Critical Care Medicine at National Jewish Health and senior co-author of the research. “This research helps advance the goal of the pulmonary community to harness macrophages in the pursuit of achieving lung repair.”
Researchers initially compared macrophage activity in two models of disease, one that was known to follow a healthy repair path and one that resulted in fibrosis, over time to determine if there were differences in the macrophage populations. The initial findings helped identify populations of responder macrophages that were recruited to the lungs in all types of lung injury. The researchers then analyzed the transcribed genes in these macrophage populations at multiple time points to better understand what differences existed.
They found that macrophages expressing Gpnmb genes, which have historically been described as “pro-fibrotic” macrophages, were found in both types of lung injury, indicating that they may not be as closely linked to fibrosis as previously thought. Further analysis found these macrophages in lung tissue samples from multiple diseases, including asthma and COVID, with a wide range of recovery outcomes. This finding prompted follow-up investigations into what led to dysfunctional healing and fibrosis in some lung diseases and not in others.
“When you take a step back and look at clinical data differently, you start to see something new,” said Alexandra McCubbrey, PhD, a researcher at National Jewish Health and senior co-author of the study. Further research into the different injury models at different time points showed that the microenvironment of the lung caused subtle changes in protein expression and macrophage survival. These changes, in the fibrotic injury model, caused distinct pathways to be activated that led the cells toward a less effective repair, as a response to the environment and external signals.
Having identified a population of macrophages that appear in all types of lung injury, and several distinct pathways that contribute to both fibrosis and to healthy repair, the researchers now plan to continue investigating what exactly triggers these differences in expression, and if it is possible to redirect macrophages that may be contributing to fibrosis to instead assist with health repair.
“Our goal is to figure out how to rebuild the injured lung,” said Dr. Janssen. His continuing research is aimed to better understand what programs macrophages and determine if they can be harnessed to encourage healthy repair even in formerly fibrotic disease.
National Jewish Health is the leading respiratory hospital in the nation. Founded in 1899 as a nonprofit hospital, National Jewish Health today is the only facility in the world dedicated exclusively to groundbreaking medical research and treatment of children and adults with respiratory, cardiac, immune, and related disorders. Patients and families come to National Jewish Health from around the world to receive cutting-edge, comprehensive, coordinated care. To learn more, visit the media resources page.
Media Resources
We have many faculty members, from bench scientists to clinicians, who can speak on almost any aspect of respiratory, immune, cardiac and gastrointestinal disease as well as lung cancer and basic immunology.
Media Contacts
Our team is available to arrange interviews, discuss events and story ideas.
- Adam Dormuth
303.398.1002 office
970.222.5034 mobile
dormutha@njhealth.org - Jessica Berry
303.398.1082 office
303.807.9491 mobile
berryj@njhealth.org
